Female Fertility Testing: Complete Diagnostic Guide and What to Expect in Chennai
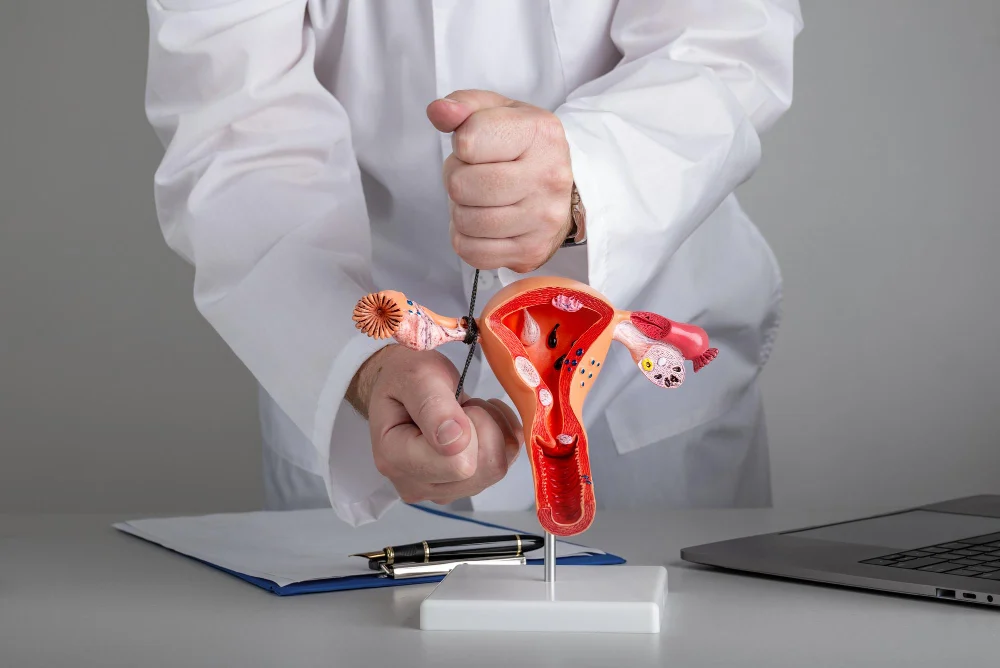
Introduction For many couples, the journey to parenthood comes with unexpected challenges. If you have been trying to conceive for over a year without success, your doctor may recommend female infertility tests to understand the underlying cause. These tests are not a cause for alarm. They are a structured, medical approach to identifying what may be affecting your fertility. Women in Perambur, Kolathur, Vyasarpadi, and across North Chennai are increasingly seeking early evaluation, which is a positive and proactive step. Understanding what fertility testing for women involves can ease anxiety and help you walk into your consultation feeling informed and prepared. What Is Female Fertility Testing? Fertility testing for women is a series of diagnostic evaluations that assess the reproductive system. The goal is to identify hormonal, structural, or ovulatory factors that may be preventing conception. These tests are usually recommended after 12 months of trying to conceive, or after 6 months if the woman is over 35. When to See a Doctor You should consult a gynaecologist if you have been trying to conceive without success for the recommended period. Earlier evaluation is advised if you have irregular or absent periods, a known history of polycystic ovary syndrome, endometriosis, thyroid disorders, or previous pelvic infections. A history of two or more miscarriages also warrants early investigation. What Tests Are Done to Evaluate Female Fertility? Hormone Blood Tests These are usually the first step in infertility diagnosis. Key hormones assessed include FSH (follicle-stimulating hormone), LH (luteinising hormone), oestradiol, prolactin, thyroid-stimulating hormone, and AMH (anti-Mullerian hormone). AMH in particular gives a reliable indication of ovarian reserve, which reflects the number of eggs remaining. Ovulation Assessment A mid-cycle progesterone blood test or serial ultrasound monitoring confirms whether ovulation is occurring regularly. Irregular cycles often suggest an ovulatory problem, which is one of the most treatable causes of female infertility. Pelvic Ultrasound A transvaginal or abdominal ultrasound evaluates the uterus, ovarian size, antral follicle count, and checks for structural issues such as fibroids, ovarian cysts, or polyps. This is a standard, non-invasive part of every fertility workup. Hysterosalpingography Known as HSG, this is an X-ray procedure that checks whether the fallopian tubes are open and whether the uterine cavity is normal. Blocked tubes can prevent eggs and sperm from meeting, and HSG helps identify this clearly. Additional Tests Depending on initial findings, a gynaecologist may recommend further evaluation such as a hysteroscopy to view the uterine cavity directly, or a diagnostic laparoscopy to assess for endometriosis or pelvic adhesions. These are performed only when clinically indicated. Srinivas Priya Hospital’s Approach to Fertility Evaluation At Srinivas Priya Hospital in Perambur, our Obstetrics and Gynaecology department provides structured, compassionate care for women undergoing fertility evaluation. We understand that this is an emotionally sensitive process, and our approach is patient-centred from the first consultation. Our gynaecologists begin with a thorough clinical history and guide each patient through the appropriate sequence of female infertility tests based on individual needs. We offer in-house diagnostic facilities including hormone blood panels, pelvic ultrasound, and gynaecological assessments, minimising the need to visit multiple locations. For women requiring further investigation such as HSG or hysteroscopy, our team coordinates these procedures with clear communication at every stage. Results are explained in simple terms so patients can make informed decisions about their next steps. Accessible from Madhavaram, Kolathur, Vyasarpadi, and the wider North Chennai area, Srinivas Priya Hospital provides quality fertility-related diagnostics within a familiar and supportive community setting. Our multi-speciality environment also ensures that related conditions such as thyroid imbalance or diabetes are managed alongside gynaecological care. Conclusion Fertility testing is a logical, medical first step when conception has been a challenge. Most causes identified through infertility diagnosis are manageable with the right treatment plan. The earlier you seek evaluation, the more options are available to you. If you are in North Chennai and have questions about your reproductive health, do not delay consultation. Compassionate, structured guidance is available at Srinivas Priya Hospital, Perambur. Taking that first step is the most important one. Frequently Asked Questions Q1: At what point should a woman consider getting female infertility tests? A woman should consider fertility testing after 12 months of trying to conceive, or after 6 months if she is over 35. If she has irregular periods, PCOS, endometriosis, or a history of miscarriage, earlier evaluation is recommended by most clinical guidelines. Q2: Are fertility tests for women painful or risky? Most female infertility tests are straightforward and low-risk. Blood tests and ultrasounds are entirely non-invasive. HSG may cause mild cramping. Procedures like hysteroscopy are done under appropriate care. Your gynaecologist will explain what to expect before each step. Q3: Can fertility issues in women be treated after diagnosis? Yes. Many causes identified through fertility testing are treatable. Hormonal imbalances, ovulation disorders, and structural issues like fibroids often respond well to medical or surgical treatment. A confirmed diagnosis allows your doctor to recommend a personalised and evidence-based care plan.